- HansJ
- 1 Comment
Three Types of Knee Pain for People. (before they become patients)
Let’s have a word about knee pain, a very common complaint in primary care clinics and in orthopaedic clinics too. More even in the Islamic world, where regular daily prayers on the knees are paramount. Therefore, it seems no surprise that Knee pain is the number-two musculoskeletal complaint. However Back pain is always the number one complaint.
- One of those pains is called patellofemoral pain syndrome, but most people don’t really know how to recognize or rather localize it.
How do we think about front Knee pain in my clinics?
Otherwise known as anterior knee pain, it’s typically caused by maltracking of the patella as the knee flexes and extends.
When I ask my patients, they will say that it’s worse when squatting, descending stairs, praying or rising from a seated position. All those actions put a lot of pressure on the joints, resulting in pain. Anterior knee pain tends not to be well characterized.
Another historical feature is the “theatergoer sign”: When you’ve been sitting for a long period of time with your knees hyper flexed, you are in agony when you stand up.
Patellofemoral pain syndrome tends to happen more in women than men because of the configuration of their joints; they have a wider so-called Q angle. It is wider because of how the hip and knee are connected in women. Wider hips pull the joint from a different angle.
I check for the theatergoer sign. It also happens in stadiums where the seats don’t provide much legroom, or long economy flights. You must curl your heels under your seat, and that pulls the patella sharply against the femur. It hurts when you stand up.
How do we treat anterior knee pain – surgery?
A chance to cut is a chance to cure. As a surgeon, I usually don’t refer these patients for surgery, if there are options to avoid it. The treatment is primarily stretching, trying to loosen things up.
Tightness is a driver of this condition, so the patient should do hamstring stretches, bringing their heel to their butt and stretching that way. We also use physiotherapy for medial strengthening with an exercise bike. There are some fancy hinge braces and boots, but it depends on your BMI or body shape if they can be of help. It’s mostly stretching and exercise. Cycling strengthens your quadriceps muscles and seems to help with the alignment.
To look for alignment problems, I might order an x-ray called the “sunrise view” or “merchant’s view,” which gives a top-down view of the kneecap, also known as “patella axial view”. The patella should be sitting between the heads of the femur, and you can tell if it tracks off to one side, or you may see jagged osteophytes, which could also cause pain.
I usually order that view. It’s nice to show a visual to the patient about what may be causing their pain.
Let’s say a patient comes into the office of a primary care physician. They heard about me and saw the social media about me all around the UAE. They are pointing to the middle of their knee, 2-3 inches below the joint line, saying, “It hurts right here.”
What might that be?
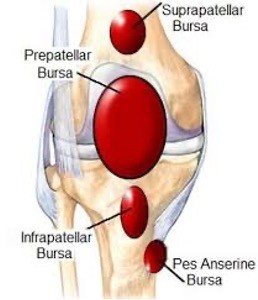
- That medial inferior to the joint line point tenderness is consistent with pes anserine bursitis. There is a bursa there. Dr Hans and others usually calls it a “bony wasteland.” You walk your fingers down and feel the bone. If you find the tender spot, then you have a pretty good idea of what’s causing the pain.
Let’s say you make the diagnosis based on palpation. It’s a straightforward diagnosis.
What can you do to help this patient?
Dr. Hans explains that there are three tendons inserting there. Two of them are hamstring tendons, so hamstring stretches can help. This type of bursitis is so close to the surface that topical NSAIDs might help. In this case, being close to the surface, topical NSAIDs might work, especially with occlusion by cling film, if you are mot allergic.
You can also get an injection of cortisone, Homeopathic or PRP. Dr. Hans has the patient indicate the point of maximal tenderness and gives the injection. Whether it’s a tendonitis or pes anserine bursitis doesn’t matter; the treatment should help.
The last thing that I want to mention, because this is a bit more vexing and complicated, is the patient who has knee pain after knee replacement.
It should be getting better;
why are they still having pain?
In his clinic Dr Hans differentiates between the patients who don’t get better and have constant pain – they are never happy with the knee replacement; and the patients who have a great initial result and then the pain recurs. It cannot be arthritis because the joint is gone. With the latter, you start thinking about potential late-stage surgical complications. Or the lack of replacing the backs side of the patella, what lot of today’s surgeons prefer for several reasons. And one can go down a deep rabbit hole as to what those might look like. Let’s focus on the patient whose pain recurs after a good result.
What kinds of things should one think about?
Could the hardware be loosening?
That can be aseptic or caused by an infection. Doc Hans orders an x-ray or a bone scan to look for lucency around the hardware. Several years after surgery, you could see activity around the implant. If you do, that would be a reason to go in and remove or revise the implant, because it’s not going to get better.
The surgeon can also determine whether it’s aseptic or infected by sending material for culture. If you don’t see any loosening on imaging, then you can get Blood Work like a CRP and ESR, which are sensitive for inflammation. If elevated, we usually aspirate and look for infection, and then you recommend antibiotics and spacers and other things that need longer explanation.
We shouldn’t forget that in this case the patient’s knee wore out, so another joint could also be worn out. We normally should look at the hip. We can do the windshield-wiper test, in which the patient sits on the edge of the table with their hips flexed at 90 degrees. You move their heel back and forth to see if that action causes hip pain. You don’t want to miss hip pain as a cause of knee pain.
Hopefully all surgeons are doing that before they just replace a knee.
But it is just true – a patient who has knee arthritis can also develop hip arthritis. You are allowed to have both, and many patients in fact do!
Kindly see an orthopedic surgeon of your choice for further questions and to find out where the origin of your Pain really is!
Physical Examination is the ONLY way to have a sincere Diagnosis and Recommendation.
Doc Hans, your orthopedic choice, is here for you.

Dr. Hans J. Poessel will carefully evaluate your injury and develop a personalized treatment plan that is right for you. He will use the latest techniques and technologies to ensure that you receive the best possible care.
To schedule an appointment with Dr. Hans, please call his office at the Number in the header and footer.
- Book an appointment with Dr. Poessel today!
I hope this blog post has been helpful for your knee pain. If you have any questions, please do not hesitate to contact me.
1 Comment
Write a Reply or Comment Cancel reply
You must be logged in to post a comment.
zoritoler imol
wonderful issues altogether, you simply won a new reader. What could you suggest in regards to your put up that you just made a few days in the past? Any certain?